Mitochondrial Disease: Understanding, Awareness, and Treatment
Mitochondrial diseases are a group of disorders caused by dysfunctional mitochondria, the organelles in cells responsible for producing energy. These diseases can affect nearly any part of the body and manifest in various ways, leading to complex and often severe symptoms. In this article, we’ll delve deep into mitochondrial disease, exploring its causes, symptoms, diagnosis, treatment, and ongoing research. We will also discuss the importance of Mitochondrial Disease Awareness Month, the color associated with the campaign, and highlight key institutions involved in treating this condition.
Mitochondrial Disease |
What is Mitochondrial Disease?
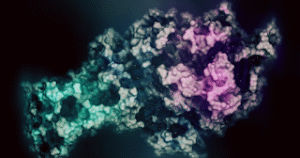
Mitochondrial disease refers to a broad range of genetic disorders that affect the mitochondria, the energy-producing structures within cells. Mitochondria are often referred to as the powerhouses of the cell because they generate most of the cell’s supply of adenosine triphosphate (ATP), used as a source of chemical energy.
Mitochondrial diseases can result from mutations in either mitochondrial DNA (mtDNA) or nuclear DNA (nDNA) that affect the function of the mitochondria. Since mitochondria are present in almost every type of cell in the body, mitochondrial diseases can affect multiple organ systems, leading to a wide variety of symptoms.
Causes of Mitochondrial Disease
Mitochondrial diseases are primarily genetic, arising from mutations in either the nuclear or mitochondrial DNA. There are two primary sources of these mutations:
- Mutations in Mitochondrial DNA (mtDNA): Mitochondria have their own DNA, separate from the nuclear DNA found in the nucleus of cells. Mutations in mtDNA are inherited maternally, meaning they are passed down from mother to child. These mutations can lead to conditions like Leigh syndrome, MELAS (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes), and LHON (Leber’s Hereditary Optic Neuropathy).
- Mutations in Nuclear DNA (nDNA): The majority of the proteins that make up the mitochondria are encoded by nuclear DNA. Mutations in nDNA that affect mitochondrial function can lead to a range of disorders. These mutations can be inherited from either parent and follow Mendelian inheritance patterns, including autosomal dominant, autosomal recessive, or X-linked inheritance.
Symptoms of Mitochondrial Disease
The symptoms of mitochondrial disease can vary widely depending on which cells in the body are affected. Since mitochondria are responsible for energy production, tissues and organs that require a lot of energy, such as the brain, heart, muscles, and liver, are often the most affected. Common symptoms include:
- Neurological Issues: Seizures, developmental delays, and neurodegeneration.
- Muscle Weakness: Myopathy, exercise intolerance, and muscle pain.
- Heart Problems: Cardiomyopathy, arrhythmias.
- Liver Disease: Liver failure or dysfunction.
- Diabetes: Often occurs in conjunction with other mitochondrial disease symptoms.
- Vision and Hearing Loss: Progressive loss of vision and hearing due to optic atrophy and sensorineural hearing loss.
- Gastrointestinal Issues: Dysmotility, severe constipation, and pseudo-obstruction.
- Respiratory Problems: Respiratory failure due to muscle weakness.
The severity of symptoms can range from mild to life-threatening, and symptoms can present at any age, from infancy to adulthood.
Diagnosis of Mitochondrial Disease
Diagnosing mitochondrial disease can be challenging due to its complexity and the wide range of symptoms it can present. A comprehensive approach is typically required, involving:
- Clinical Evaluation: A detailed medical history and physical examination are crucial. Physicians look for common signs of mitochondrial disease, such as muscle weakness, neurological issues, and organ dysfunction.
- Genetic Testing: This is the most definitive method for diagnosing mitochondrial disease. Next-generation sequencing (NGS) can identify mutations in mtDNA or nDNA that affect mitochondrial function.
- Biochemical Testing: Tests such as blood lactate levels, cerebrospinal fluid (CSF) lactate, and pyruvate levels can indicate mitochondrial dysfunction.
- Muscle Biopsy: A muscle biopsy may be performed to assess the structure and function of mitochondria within muscle tissue. This can include histological examination and enzymatic assays to measure mitochondrial respiratory chain activity.
- Imaging: MRI or CT scans may be used to assess brain structure and identify abnormalities that could be related to mitochondrial disease, such as lesions or brain atrophy.
Treatment of Mitochondrial Disease
Currently, there is no cure for mitochondrial disease, and treatment focuses on managing symptoms and improving quality of life. A multidisciplinary approach is often necessary, involving various specialists depending on the organs affected. Treatment strategies may include:
- Medications: Certain medications can help manage symptoms, such as anticonvulsants for seizures, insulin for diabetes, and medications for heart conditions.
- Nutritional Support: Some patients benefit from specific vitamins and supplements that support mitochondrial function, such as Coenzyme Q10, L-carnitine, and B vitamins.
- Physical Therapy: Physical and occupational therapy can help maintain muscle strength and function.
- Surgery: In some cases, surgical interventions may be necessary to address complications, such as pacemaker implantation for arrhythmias or feeding tubes for gastrointestinal dysfunction.
- Gene Therapy: Research is ongoing into potential gene therapy approaches that could correct the underlying genetic defects in mitochondrial disease. This area of research is still in its early stages but offers hope for future treatments.
Ongoing Research and Future Directions
Research into mitochondrial disease is ongoing, with scientists exploring various avenues to better understand and treat these complex disorders. Some key areas of research include:
- Gene Therapy: Researchers are investigating ways to deliver healthy copies of genes to cells with defective mitochondria. This approach has shown promise in animal models, and clinical trials are ongoing.
- Mitochondrial Replacement Therapy (MRT): MRT is a technique that involves replacing defective mitochondria in an egg or embryo with healthy mitochondria from a donor. This technique is still experimental but has the potential to prevent the transmission of mitochondrial diseases from mother to child.
- Drug Development: Scientists are working to develop new drugs that can improve mitochondrial function or compensate for mitochondrial dysfunction. Some of these drugs are currently in clinical trials.
- Stem Cell Therapy: Researchers are exploring the use of stem cells to repair or replace damaged tissues in patients with mitochondrial disease.
Mitochondrial Disease Awareness Month
Mitochondrial Disease Awareness Month is observed every September, dedicated to raising awareness about mitochondrial diseases and supporting those affected by these conditions. The campaign is crucial in promoting understanding, funding research, and advocating for better treatments and support for patients and families.
The Color of the Campaign
The color associated with Mitochondrial Disease Awareness Month is green. This color symbolizes the vitality and energy that mitochondria provide to our cells and the hope for a cure in the future. During this month, various events and activities are organized worldwide to spread awareness, including walks, fundraisers, and educational seminars.
Key Institutions for Mitochondrial Disease Treatment
Several institutions around the world are at the forefront of mitochondrial disease research, diagnosis, and treatment. These institutions provide comprehensive care and support for patients and their families.
Cleveland Clinic
Cleveland Clinic Mitochondrial Disease Program
The Cleveland Clinic offers a specialized program dedicated to diagnosing and treating mitochondrial diseases, providing access to expert care and the latest research.
Children’s Hospital of Philadelphia (CHOP)
CHOP Mitochondrial Medicine
CHOP’s Mitochondrial Medicine program is a leader in the field, offering cutting-edge diagnostic and therapeutic options for children with mitochondrial disorders.
National Institute of Neurological Disorders and Stroke (NINDS)
NINDS Mitochondrial Disorders
NINDS conducts and supports research on mitochondrial diseases, working to uncover the underlying mechanisms and develop new treatments.
Boston Children’s Hospital
Boston Children’s Hospital Mitochondrial Program
This program provides comprehensive care for children with mitochondrial disorders, including genetic counseling, diagnostic services, and treatment.
University of Melbourne Mitochondrial Disease Research
UMDF Mitochondrial Disease Research
The University of Melbourne is involved in extensive research on mitochondrial diseases, focusing on understanding the genetic basis of these conditions and developing new therapies.
The Lily Foundation
The Lily Foundation
The Lily Foundation is a UK-based charity dedicated to supporting patients and families affected by mitochondrial disease, funding research, and raising awareness.
Mito Foundation
Mito Foundation
The Mito Foundation in Australia provides support to those affected by mitochondrial disease and funds research into new treatments and potential cures.
MitoAction
MitoAction
MitoAction supports individuals and families affected by mitochondrial disease through education, advocacy, and support services. They also organize events to raise awareness and funds for research.
United Mitochondrial Disease Foundation (UMDF)
UMDF
The UMDF is dedicated to promoting research, providing support for families, and raising awareness about mitochondrial diseases. They organize World Mitochondrial Disease Week to engage the public and increase understanding of these conditions.
National Center for Biotechnology Information (NCBI)
NCBI Mitochondrial Disease Information
NCBI provides comprehensive information on mitochondrial diseases, including detailed scientific and clinical insights into the various conditions.
Conclusion
Mitochondrial diseases represent a complex and diverse group of disorders that impact many aspects of health and quality of life. Although there is currently no cure, advancements in research, diagnostics, and treatments offer hope for better management and potential future therapies. Awareness campaigns such as Mitochondrial Disease Awareness Month play a crucial role in increasing understanding, supporting affected individuals and families, and driving forward the search for a cure.
By recognizing the symptoms, understanding the underlying causes, and supporting ongoing research, we can contribute to improving the lives of those affected by mitochondrial diseases and ultimately finding effective treatments and solutions.
